Diabetic Eye Diseases
Diabetic eye disease refers to a group of eye problems that people with diabetes may face. Fortunately, diabetic eye disease often can be treated before vision loss occurs but all diabetic eye diseases can cause severe vision loss and even blindness.
We recommend that everyone who has diabetes has a dilated eye exam at least once a year to stay ahead of diabetic eye diseases.
Diabetic eye diseases include:
- Diabetic retinopathy
- Cataracts
- Glaucoma
Diabetic Retinopathy
Diabetic retinopathy is the most common eye disease in people with diabetes.
What is diabetic retinopathy?
Diabetic retinopathy is an eye disease that causes blindness in adults.
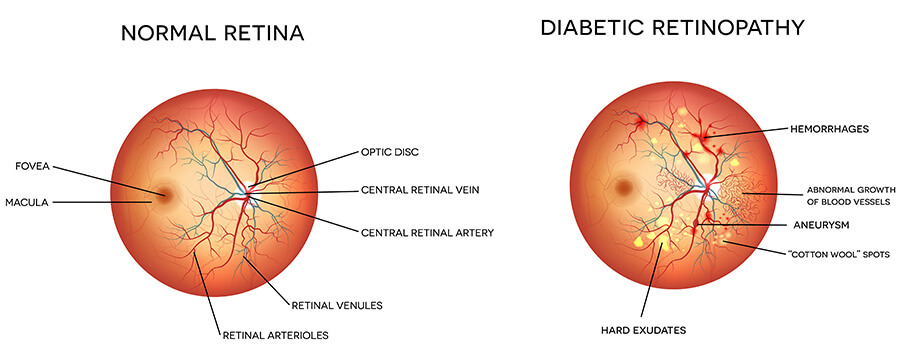
Diabetic retinopathy can be caused by changes in the blood vessels of your retina and changes in the light sensitive layer of tissue at the back of your inner eye.
There are two stages of diabetic retinopathy:
Non-proliferative retinopathy- This is the early stage of the disease where blood vessels swell and leak. This causes a swelling of your retina or macular edema. Macular edema may result in mild vision loss.
Proliferative retinopathy – This is the advanced stage of the disease where abnormal new blood vessels grow on the surface of your retina. These vessels may break and bleed into the vitreous and cause severe vision loss.
You can reduce your risk of getting diabetic retinopathy even though you can not completely prevent diabetic retinopathy. Controlling your blood sugar slows your eyes from getting retinopathy, keeps it from getting worse and lessens the need for laser surgery for severe retinopathy.
What causes diabetic retinopathy?
Changes in the blood vessels of the retina cause diabetic retinopathy.
In some people with diabetic retinopathy, the blood vessels in the retina may swell and leak fluid. In others, abnormal new blood vessels grow on the surface of the retina. These changes may result in vision loss or blindness.
Who is at risk for diabetic retinopathy?
Anyone with diabetes is at risk for diabetic retinopathy. The longer you have diabetes, the more likely you are to develop diabetic retinopathy. Your risk rises if you have diabetes and you smoke, have high blood pressure, or are pregnant.
What are the symptoms of diabetic retinopathy?
In the early stages of diabetic retinopathy, you may have no symptoms. Vision may not change until the disease gets worse. Then you may have blurry or double vision, dark or floating spots, pain or pressure in one or both eyes, rings, flashing lights, or blank spots in your vision.
A condition called macular edema may occur from diabetic retinopathy. It happens when the macula, a part of the retina, swells from the leaking fluid and causes blurred vision. When new vessels grow on the surface of the retina, they can bleed into the eye. This may decrease vision.
How is diabetic retinopathy diagnosed?
Along with a complete health history and eye exam, your eye doctor may do these tests to diagnose diabetic retinopathy:
- Visual acuity test – This is the common eye chart test. It measures vision ability at various distances.
- Tonometry – This standard test is done to check the pressure (intraocular pressure, or IOP) inside the eye.
- Pupil dilation – For a close up exam of the eye’s lens and retina, your pupil is widened with eye drops.
- Ophthalmoscopy – This is a test where a doctor looks very closely at the retina using a special magnifying glass.
- Fluorescein angiography – In this test, a dye is injected into the bloodstream. The dye helps the blood vessels in the eye show up while pictures are taken with a special camera. This test lets the doctor see if the blood vessels are leaking.
- Optical coherence tomograph – In this test, light waves are used to make detailed images of the retina.
How is diabetic retinopathy treated?
Your treatment will depend on your symptoms, age, and general health and how severe your condition is.
Even people with advanced retinopathy have a good chance of keeping their vision if they are treated before the retina becomes severely damaged.
Treatment for diabetic retinopathy may include:
Laser surgery – Laser surgery is often used to treat macular edema and proliferative retinopathy. It involves shrinking the abnormal blood vessels or sealing the leaking ones.
Vitrectomy – Vitrectomy is a procedure that involves removing the cloudy, jelly-like substance (vitreous) that fills the center of the eye. the vitreous is replaced with a saline solution.
Injections – Certain chemicals can be injected into the eye to slow the growth of the abnormal vessels of the retina.
Can diabetic retinopathy be prevented?
Although you can’t prevent diabetic retinopathy, you can reduce the risk of developing by:
- Having a dilated eye exam once a year. An eye exam does not prevent retinopathy. But it can help diagnose eye problems that can then be treated. An eye exam can also alert you and your healthcare provider if diabetes needs to be better controlled.
- If you’re a woman with diabetes, have an eye exam before pregnancy or in the first trimester. Continue to be monitored every trimester and for 1 year after birth depending on how severe the retinopathy is.
Follow your diabetes management plan by:
- Taking medicines as directed
- Using insulin as directed, if needed
- Eating to manage blood sugar level
- Exercising to lower and help the body use blood sugar
- Testing blood-sugar levels regularly
- Testing urine for ketone levels regularly
- Regular healthcare follow-up to evaluate diabetes control and rule out or treat other risk factors, such as high blood pressure
We can’t stress enough that better control of blood sugar slows the onset and progression of retinopathy and lessens the need for laser surgery for severe retinopathy.
Key Points
- Changes in the blood vessels of the retina cause diabetic retinopathy. Retinal blood vessels may swell and leak fluid or new blood vessels may grow on the surface of the retina. These changes may result in vision loss or blindness
- Anyone with diabetes is at risk for diabetic retinopathy. The longer you have diabetes, the more likely you are to develop diabetic retinopathy.
- Treatment for diabetic retinopathy may include laser surgery, vitrectomy, and injection of chemicals to stop new blood vessels from forming.
- Better control of blood sugar slows the start and progression of retinopathy. It also lessens the need for laser surgery for severe retinopathy.
Next Steps
Tips to help you get the most from your visit:
- Know the reason for your visit and what you want to happen.
- Before your visit, write down the questions you want answered.
- Bring someone with you to help you ask questions and remember what your provider tells you.
- At the visit, write down the name of a new diagnosis, and any new medicines, treatments, or tests. Also, write down any new instructions your provider gives you.
- Know why a new medicine or treatment is prescribed, and how it will help you. Also, know what the side effects are.
- Ask if your condition can be treated in other ways.
- Know why a test or procedure is recommended and what the results could mean.
- Know what to expect if you do not take the medicine or have the test or procedure.
- If you have a follow-up appointment, write down the date, time, and purpose for that visit.
- Know how you can contact your provider if you have questions.
Age-Related Macular Degeneration Definition
Age-related macular degeneration is the most common cause of severe loss of eyesight among people 50 and older. Only the center of vision is affected by this disease. It is important to realize that people rarely go blind from it.
AMD affects the central vision, and with it, the ability to see fine details. In AMD, a part of the retina called the macula is damaged. In advanced stages, you can lose your ability to drive, to see faces, and to read smaller print. In its early stages, AMD may have no signs or symptoms, so you may not suspect they have it.
Types of Age-Related Macular Degeneration and Causes
The two primary types of age-related macular degeneration have different causes:
Dry. This type is the most common. About 80% of those with AMD have the dry form. Its exact cause is unknown, although both genetic and environmental factors are thought to play a role. This happens as the light-sensitive cells in the macula slowly break down, generally one eye at a time. The loss of vision in this condition is usually slow and gradual. It is believed that the age-related damage of an important support membrane under the retina contributes to dry age-related macular degeneration.
Wet. Though this type is less common, it usually leads to more severe vision loss in patients than dry AMD. It is the most common cause of severe loss of vision. Wet AMD happens when abnormal blood vessels start to grow beneath the retina. They leak fluid and blood — hence the name wet AMD — and can create a large blind spot in the center of the visual field.
Risk Factors for Age-Related Macular Degeneration
There are several risk factors that can contribute to developing age-related macular degeneration, including:
- Being 50 and older
- Eating a diet high in saturated fat
- Smoking
- High blood pressure or hypertension
Age-Related Macular Degeneration Symptoms
The following are the most common symptoms of age-related macular degeneration. However, each individual may experience symptoms differently.
Symptoms may include:
- Blurry or fuzzy vision
- Difficulty recognizing familiar faces
- Straight lines appear wavy
- A dark, empty area or blind spot appears in the center of vision
- Loss of central vision, which is necessary for driving, reading, recognizing faces and
performing close-up work
The presence of drusen, which are tiny yellow deposits in the retina, is one of the most common early signs of age-related macular degeneration. It may mean the eye is at risk for developing more severe age-related macular degeneration. These will be visible to your doctor during an eye exam.
The symptoms of age-related macular degeneration may look like other eye conditions. Speak with an eye care professional for diagnosis.
Age-Related Macular Degeneration Diagnosis
In addition to a complete medical history and eye exam, your eye doctor may do the following tests to diagnose age-related macular degeneration:
Visual acuity test. This common eye chart test measures vision ability at various distances.
Pupil dilation. The pupil is widened with eye drops to allow a close-up examination of the eye’s retina.
Fluorescein angiography. Used to detect wet age-related macular degeneration, this diagnostic test involves a special dye injected into a vein in the arm. Pictures are then taken as the dye passes through the blood vessels in the retina, helping the doctor evaluate if the blood vessels are leaking and whether or not the leaking can be treated.
Amsler grid. Used to detect wet age-related macular degeneration, this test uses a checkerboard-like grid to determine if the straight lines in the pattern appear wavy or missing to the patient. Both indications may signal the possibility of age-related macular degeneration.
Amsler Grid
To use the Amsler grid, follow these steps:
- Wearing any glasses you normally use to read, hold the grid 12 to 15 inches away from your face in good light.
- Cover one eye.
- Look directly at the center dot with your uncovered eye and keep your eye focused on it.
- While looking directly at the center dot, notice in your side vision if all grid lines look straight or if any lines or areas look blurry, wavy, dark or blank.
- Follow the same steps with the other eye.
If you notice any areas of the grid that appear darker, wavy, blank or blurry, contact us right away.
Age-Related Macular Degeneration Treatment
Specific treatment for age-related macular degeneration will be determined by your eye MD based on:
- Your age, overall health and medical history
- Extent and nature of the disease
- Your tolerance for specific medications, procedures or low-vision therapies
- Expectations for the course of the disease
- Your opinion or preference
Currently, there is no treatment for dry age-related macular degeneration, though vision rehabilitation programs and low-vision devices can be used to build visual skills, develop new ways to perform daily living activities and adjust to living with age-related macular degeneration.
The main treatment for wet AMD is the injection of medications called anti-VEGF agents. VEGF stands for vascular endothelial growth factor. A high level of VEGF in the eye is linked to the formation of the abnormal blood vessels that cause much of the damage in wet AMD. Anti-VEGF agents are used to combat the disease process and reduce the damaging effects of these leaky abnormal blood vessels. They are also able to effectively stabilize vision in many patients.
In some patients, anti-VEGF injections actually improve the level of visual acuity. Anti-VEGF medications are administered by injecting them directly into the affected eye. Although this sounds daunting, the procedure is done with a very fine needle and under the cover of numbing (anesthetic) eye drops, so patients are usually very comfortable. Anti-VEGF treatment is usually administered regularly over time, requiring multiple injections to maintain the treatment effect, and your retinal physician will discuss the best treatment schedule for you. In selected patients, other treatments, such as laser therapy, can be used, if necessary.
Complications of Age-Related Macular Degeneration
Age-related macular degeneration can result in severe loss of central vision but rarely causes blindness. It can, however, make it difficult to read, drive or perform other daily activities that require fine central vision. In AMD, the health of the peripheral retina is unaffected, so patients can rest assured that their peripheral (side) vision, and their ability to walk around without bumping into things, is usually preserved.
Please reach out to us at 860 644-5011 if you have any questions or suspect you may have Age-Related Macular Degeneration.




